Definition
Irritable bowel syndrome (IBS) is a common disorder that affects the large intestine (colon). Irritable bowel syndrome commonly causes cramping, abdominal pain, bloating, gas, diarrhea and constipation. IBS is a chronic condition that you will need to manage long term.
Only a small number of people with irritable bowel syndrome have severe signs and symptoms. Some people can control their symptoms by managing diet, lifestyle and stress. Others will need medication and counseling.
Symptoms
The signs and symptoms of irritable bowel syndrome can vary widely from person to person and often resemble those of other diseases. Among the most common are:
- Abdominal pain or cramping
- A bloated feeling
- Gas
- Diarrhea or constipation — sometimes alternating bouts of constipation and diarrhea
- Mucus in the stool
For most people, IBS is a chronic condition, although there will likely be times when the signs and symptoms are worse and times when they improve or even disappear completely.
Symptoms that may indicate a more serious condition include:
- Rectal bleeding
- Abdominal pain that progresses or occurs at night
- Weight loss
MIND: Tailored Gut directed Hypnotherapy for IBS
Hypnosis has been shown to be an effective treatment for irritable bowel syndrome (IBS) in a number of clinical studies. Hypnotherapy for IBS involves progressive relaxation, and then suggestions of soothing imagery and sensations focused on the individual’s symptoms. Improvements in overall well-being, quality of life, abdominal pain, constipation, diarrhea, and bloating have been noted.
Contrary to many portrayals in fiction, a clinical hypnotherapist has no power over the hypnotized person. The person is typically aware of what happens both during and after the hypnosis session. The treatment is generally comfortable and also can be effective when people are treated in groups.
Research has found that hypnotherapy may help improve the primary symptoms of IBS. It may also help relieve other symptoms suffered by many people with IBS such as nausea, fatigue, backache, and urinary problems. Hypnotherapy appears to offer symptomatic, psychological, and physiological benefit.
However, hypnosis should not be regarded as a cure-all. Up to 25% of patients fail to respond. Even when people do improve, conventional approaches to treatment should not always be ignored. It is still important that lifestyle factors such as diet are also taken into account. In addition, some people may find that an occasional loperamide or laxative, depending on the bowel habit abnormality, may be required.
Do the effects of hypnotherapy last once a course of treatment has been completed?
Research on the long-term follow up of patients who have benefited shows that after a period of between 1 and 5 years, most remain well with many requiring no further medication at all.
Hypnotherapy can be a time-consuming and costly approach in the short term. However, as a result of the sustained benefits of treatment, it has been calculated that it becomes cost effective within 2 years when compared to conventional approaches.
How to Select a Hypnotherapist?
1) Does this person have formal training and significant experience in clinical hypnosis and psychology field? Using hypnosis with good success requires considerable skill and knowledge. In general, 50 hours or more of certified workshop training in hypnosis would be good, although less is sometimes adequate.
2) Does this person know the details of successful hypnosis treatment protocols for IBS? Hypnosis in itself is probably not sufficient to treat IBS effectively. Specific gut-directed hypnotherapy method need to be included.
Summary
Hypnosis is just one of many in the treatment options for IBS. Other psychological methods, cognitive therapy in particular, are also effective options. Hypnosis may be especially suitable when severe chronic symptoms continue after standard medical management approaches have been tried. It has become clear that in such cases, hypnosis treatment can often produce major improvement that can last for years.
Research about how clinical hypnotherapy can help Irritable Bowel Syndrome:
The Efficacy of Hypnotherapy in the Treatment of Irritable Bowel Syndrome: A Systematic Review and meta-analysis
This study provides clearer evidence that hypnotherapy has beneficial short-term effects in improving gastrointestinal symptoms of patients with IBS.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4015203/
Efficacy, tolerability, and safety of hypnosis in adult irritable bowel syndrome: systematic review and meta-analysis.
This meta-analysis demonstrated that hypnosis was safe and provided long-term adequate symptom relief in 54% of patients with irritable bowel syndrome refractory to conventional therapy.
http://www.ncbi.nlm.nih.gov/pubmed/24901382
BRAIN Perspective: EEG biofeedback for IBS
Individuals who suffer from Irritable Bowel Syndrome (IBS) may experience a range of symptoms, from mild annoyance to severe, debilitating distress. Symptoms can range from chronic, mild dysregulation of gut motility to episodes of diarrhea or constipation that incapacitate the patient and cause loss of time at work, withdrawal from family activities, and even hospitalization. It is estimated that about 20% of North Americans suffer from IBS, with twice as many women than men diagnosed each year.
Research in neuroscience has revealed that the intestinal tract and the brain are intimately related in terms of hormonal activity and autonomic nervous system connections. This is referred to as the "Gut-Brain Connection." Individuals with IBS frequently present with evidence of abnormal high frequency brain wave activity in the frontal lobes where emotional regulation occurs.
These unbalanced brain waves can be altered with Neurofeedback training (see box on right) to correct the abnormal activity and either partially or completely relieve the symptoms of IBS.
Neurotherapy/EEG biofeedback training begins with a brain assessment procedure to locate the sources of unbalanced brain wave activity. Following this, training begins and may last for 10 to 15 sessions. Each session may last for 30-40 minutes. We use symptom checklists, clinical history and patient reports to assess the progress of treatment.
How it works?
EEG biofeedback training for Irritable Bowel Syndrome (IBS) is a way of learning how to control your brain's electrical activity in order to alleviate the distress of IBS. EEG biofeedback training can significantly reduce or even eliminate IBS symptoms and painful sensations in patients who have an underlying dysregulation of the Autonomic Nervous System ("Fight/Flight/Freeze" emotional response).
The technique is simple and painless: Brainwave sensors are attached to the scalp at strategic locations and the information from the brain is processed digitally with sophisticated computer programs. Audio or visual displays give feedback to the patient about the frequency and amplitude of the brain activities that are implicated in IBS sensations. Music or video feedback allows the patient to become successful in changing the brain wave patterns and as a result, the IBS is greatly relieved or eliminated.
What is EEG biofeedback?
EEG biofeedback training is a simple, painless learning technique that involves teaching your brain waves to become more functional and effective. The most comprehensive definition of EEG biofeedback comes to us from the International Society for Neurofeedback and Research (ISNR). Go to www.ISNR.net for more information.
EEG biofeedback does not involve either surgery or medication and is neither painful nor embarassing. When provided by a licensed professional with appropriate training, generally trainees do not experience negative side-effects. Typically trainees find NFT to be an interesting experience. EEG biofeedback training operates at a brain functional level and transcends the need to classify using existing diagnostic categories. It modulates the brain activity at the level of the neuronal dynamics of excitation and inhibition which underly the characteristic effects that are reported.
Research demonstrates that EEG biofeedback is an effective intervention for ADHD and Epilepsy. Ongoing research is investigating the effectiveness of EEG biofeedback for other disorders such as Autism, headaches, insomnia, anxiety, substance abuse, TBI and other pain disorders, and is promising.
.jpg)
大腸激躁症
腹脹、腹鳴、腹瀉、便秘、肚子疼痛不適,大概是所有人都曾經驗過的症狀,但許多人無論怎麼吃藥、看醫師,問題就是無法改善,每天都得面臨不斷跑廁所、或「大」不出來的痛苦,這些人都是大腸激躁症(Irritable Bowel Syndrome)的受害者。大腸激躁症,或稱為大腸急躁症、腸躁症、刺激性腸症候群、急躁性腸症候群、腸躁症候群,指的都是一種腸道的功能性異常;就和其五花八門的中文譯名一樣,這種疾病的症狀也相當複雜,有人易腹瀉、有人易便秘、有人則腹瀉與便秘交錯發生。
台北新光醫院胃腸肝膽科醫師劉玉華指出,在幽門螺旋桿菌可藉藥物治療後,以往腸胃科門診最常見的消化性潰瘍已減少,取而代之的是大腸激躁症,幾乎半數病患都因這種功能性障礙來求診;據估計,一到兩成的人口有此困擾;在國外,這更是僅次於感冒、最常造成職場請假的疾病。劉玉華表示,大腸激躁症的病因至今不明,幾乎所有找不到原因的腸胃功能障礙,都可歸到其名下。
但這種病症有幾個共通特點,一是會反覆發生、屬於慢性問題;第二,不會合併血便、黑便、發燒等其他症狀;三,不影響營養吸收,體重不會減輕。值得一提的是,這種病常有在特定情況下發作的特性,例如,有些人喝了酒、吃太飽、吃了麻辣鍋、甚至吃冰後就發作;有人吹了風、睡醒後、考試期間、工作時容易發作,有人出國旅行時症狀即消失,有人則在休假時症狀反加重。
醫師分析,雖然有些病人可能是體質所致、從小就有這種腸道功能障礙,但更多人可能是壓力所引起,因此正忙於打拼事業、照顧家庭的青壯年族群,最常見發病,且以女性為多,有些患者則有易憂鬱、易焦慮、愛鑽牛角尖、追求完美等人格特質。不過,大腸激躁症的患者雖多,調查卻發現,四分之三的病人都未就醫,可能是許多人認為,大號不通暢只小問題,忍一忍就過去,未予多注意。但另一方面,也有不少病患因症狀持續,四處就醫、接受各種檢查,耗費許多醫療資源,據統計,國內每年消化不良造成的健保花費達九十億元,可見大腸激躁症不僅是惱人的毛病,也是相當花錢的疾病。
大腸激躁症的症狀是什麼?
1. 腹部絞痛
2. 腹部脹氣、鼓脹
3. 腹瀉、便秘、或腹瀉與便秘交互出現
4. 常與情緒反應有關,如工作忙碌時、重大考試前都會加重症狀
5. 雖長期受腸胃症狀困擾,通常體重並不會減輕,也不會有嚴重的併發症
大腸激躁症如何治療?
1. 要先就醫檢查,排除其他症狀相似的疾病,如:乳糖耐受不良、大腸癌等。
2. 調適心理、適應壓力,若是可能盡量避免給自己太過的壓力。
3. 正常的作息,規律的運動。
4. 避免刺激性的飲食,如:菸、酒、咖啡、茶葉等。
5. 攝取足量的高纖維性食物。
6. 若症狀仍持續,應考慮調整神經傳導物質,以恢復自律神經之正常生理功能。
大腸激躁症是腸胃科疾病嗎?
大腸激躁症不是『器質性腸胃科疾病』,而是屬於『功能性疾病』( functional disorder )之一』。---所有功能性疾病皆由『自律神經失調』所引起,自律神經系統分佈至各內臟器官,管理各內臟器官的功能運作,一旦自律神經失調,則其所調控的內臟出現其相關疾病(例如:大腸激躁症 )。所以,大腸激躁症的治療不能從腸胃科取向去做,應從自律神經取向方能治本。
如何改善症狀?僅記以下數個原則:
1. 改變飲食習慣:不談公事、輕鬆進食、細嚼慢嚥。
2. 改變食譜:不吃乳製品、油脂食物、酒精、咖啡因的飲料。食物力求低脂、少糖、少鹽、適度的蛋白質、高纖維食物。
3. 生活減壓:壓力與腸子的蠕動有密切的關係。尤其每天在壓力鍋當中打滾的人們,更是有機會罹患大腸激躁症。每天工作八小時當中,找空檔舒緩身心。勤練肌肉鬆弛術、靜坐,平衡身心靈。
4. 天天運動:運動除了強身之外,更可以放鬆心情,消除鬱悶的情緒,強化腸胃的機能。
5. 正常的作息、充足的睡眠。
6. 改變個性:完美主義的人,容易給自己壓力,也常出現焦慮、憂鬱或身心症狀。所以改變對事物的看法與態度,降低標準,隨遇而安,腸胃自然沒承受太多的壓力。
7. 尋找適當的醫療:激躁性腸症並非一般拉肚子,幾天就可以康復的 。必須有耐心的就醫,配合腸胃科與精神科藥物方能奏效。
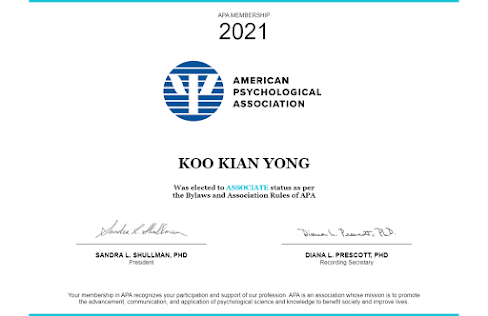
(Clinical Hypnotherapist Hiro Koo: 催眠在临床研究上,临床催眠对IBS大腸激躁症的疗效是受承认和备受肯定的。)
Source:
http://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/basics/definition/CON-20024578
http://www.cs.nthu.edu.tw/~dr824349/personal/article/IBS.html
http://norcalneurotherapy.com/neurofeedback-for-ibs.php
http://www.aboutibs.org/site/treatment/complementary-or-alternative-treatments/hypnosis






.jpg)